Lumbar Spine Manipulation
I (Steve) thought I would discuss the clinical prediction rule for manipulation of the lumbar spine. Although an old study, it had a significant influence on how manipulation is practiced and the clinical decision-making behind the intervention. It has also been scrutinized and misinterpreted frequently over the last decade.
First a little background. In 2002, Tim Flynn took 71 patients with low back pain (LBP) and prospectively tested them on a number of variables from both the history and the clinical examination. He then treated all patients with two sessions of lumbar spinal manipulative therapy (SMT) over a one week period. The treatment effect was dichotomized as success or non-success based on a 50% reduction in Oswestry Disability Index (ODI) score. Those patients considered a success were further analyzed to determine common factors the patients shared from the history and the clinical examination. Noteworthy is that 45% of all patients who received lumbar SMT demonstrated the 50% improvement. In addition no adverse events were reported.
Factors associated with success included:
Pain lasting less than 16 days
No symptoms distal to the knee
FABQ score less than 19
Internal Rotation of greater than 35 degrees for at least one hip
Hypomobility of a least one level of the lumbar spine
Having 4/5 of these variables positive increased the likelihood of dramatic success to 95%. Interestingly, Tim Flynn was a highly touted manual therapist and fully believed in a biomechanical model and thought that this study would provide evidence for this form of clinical reasoning. Tim now refers to himself as a recovering biomechanist!
John Childs then prospectively tested the rule in a randomized controlled trial with four groups: 1) patients positive on the CPR who received two manipulations and three sessions of stability exercises, (2) patients positive on the rule who received five sessions of exercise based therapy, (3) patients negative on the rule and received manipulation and stabilization exercises, and (4) patients negative on the rule and received five sessions of exercise based therapy.
Those patients positive on the rule who received manipulation demonstrated dramatic improvements compared to those positive on the rule who only received the exercise based therapy. It is worth noting that these effects were not only dramatic but also long lasting. At six month follow-up as demonstrated by the graph below:
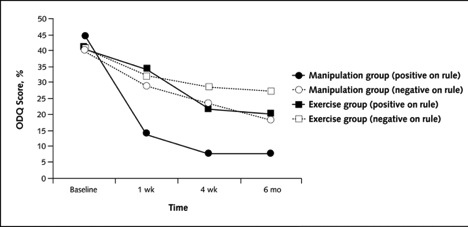
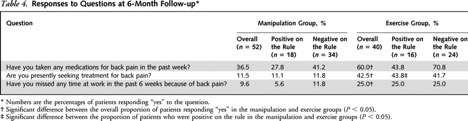
Furthermore, the benefits were not limited to just improvement in ODI scores; at six month follow-up, those patients receiving manipulation demonstrated a reduction in the use of medication, utilization of treatment, and lost time from work. Again, no adverse events were reported.
Although the CPR is helpful at identifying a sub-group of responders to lumbar SMT, isn’t there a faster maybe more pragmatic screening exam? Well Fritz. et al examined the variables that were predictive of success with lumbar SMT. The authors took the 71 subjects used to develop the CPR (1) and the 70 subjects randomized to receive the manipulation intervention taken from the validation study (2) and found that with the two criteria present - acute low back pain (less than 16 days) and no symptoms distal to the knee - yielded a positive likelihood ratio of 7 (95% CI: 3.2-16.1) (3). That is, patients were 7 times more likely to have a favorable response (a 50% reduction in the ODI score) to lumbar SMT if these two criteria were present.
“For those positive on the rule, spinal manipulation appears to have a “Slam dunk” effect and is perhaps considered negligent to potentially withhold the intervention.”
For those positive on the rule, spinal manipulation appears to have a “Slam dunk” effect and is perhaps considered negligent to potentially withhold the intervention. If we look more closely at the data, patients in the manipulation group demonstrated significantly better results in outcomes at six weeks irrespective of status on the prediction rule when compared to those only receiving exercise - although the effect size was not as dramatic. On this basis, perhaps our clinical question should not be “Who should we manipulate” but rather “Who shouldn’t we manipulate”.
I hope this provides stimulus for thought and I encourage you to review these two studies and reflect about how the information should effect your practice.
Happy Reading!
Authors
References
Childs, John D., et al. "A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. "Annals of internal medicine." 141.12 (2004): 920-928.
http://annals.org/article.aspx?articleid=718023
Flynn, Timothy, et al. "A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation."Spine 27.24 (2002): 2835-2843.
http://fearonphysicaltherapy.com/_media/media/file/342138/ManipCPR-Flynn-Development.pdf
Fritz, Julie, et al. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. “BMC Family Practice. (2005) 6:29.
STEVE YOUNG, BSCPT, BA

SEAN OVERIN, BHK, MPT


