Imaging and the Lumbar Spine: What does it tell us?
By Sean Overin BHK, MPT, DPT & Steve Young BA, BHSc PT, DPT

Traditionally, a pathoanatomical approach has been used in medicine in order to guide treatment intervention; a specific pathology is identified and based on this disease a specific treatment intervention is implemented. It has been estimated that 65-80% of the population will experience at least one episode of low back pain (LBP)1, and unfortunately, there is evidence we are unable to accurately identify the specific cause for the vast majority of these patients2.
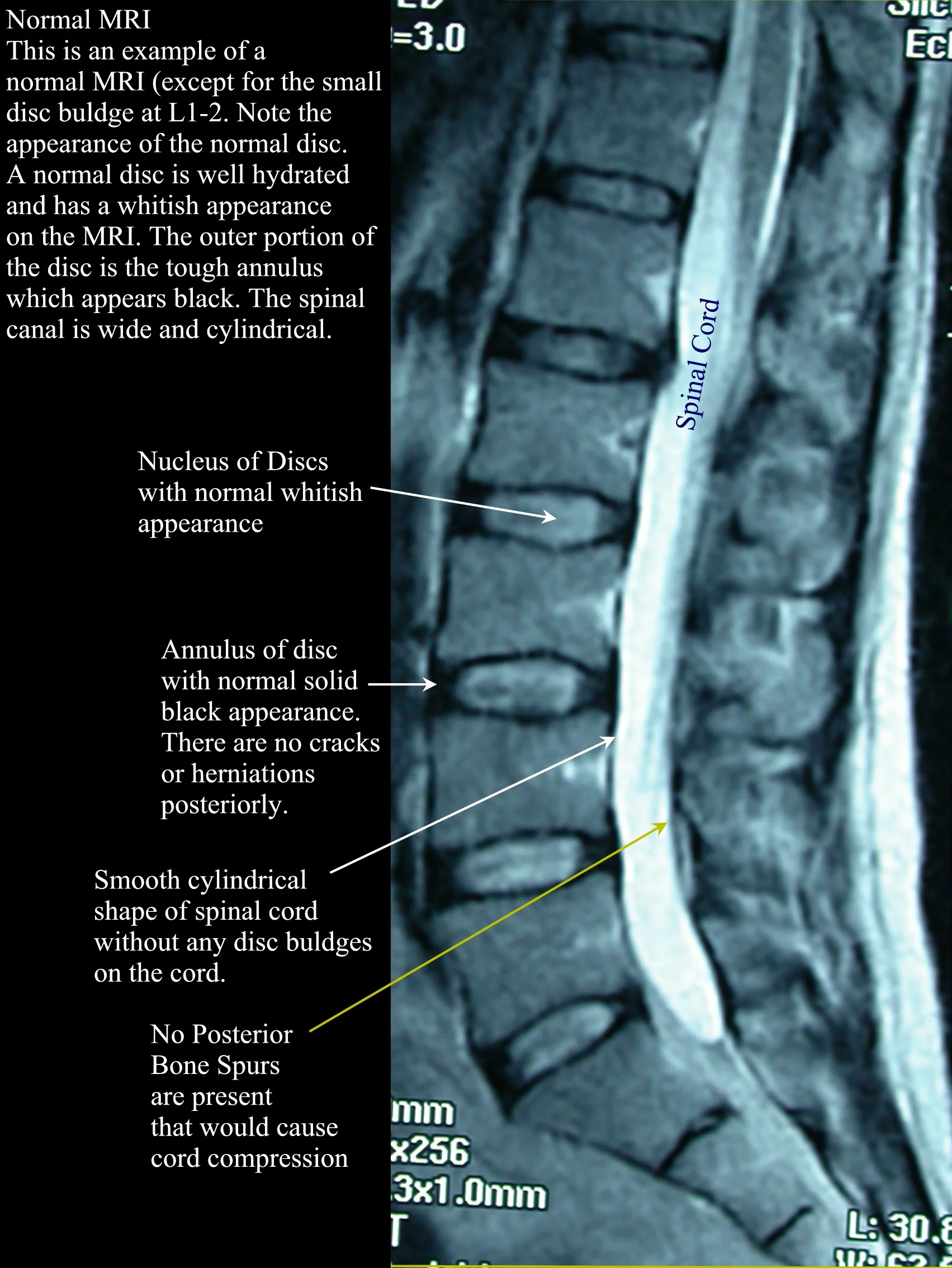
In a classic study published in the New England Journal of Medicine, 98 asymptomatic individuals had magnetic resonance imaging (MRI) of their lumbar spine and over 60% presented with some type of abnormality according to the reading radiologist3. In another study, a prospective cohort of patients without LBP were given an MRI and a multitude of self-report questionnaires then followed for three years to determine factors associated with the development of LBP4. Similar incidences of asymptomatic findings were found on MRI as was seen in the New England Journal of Medicine study. The only anatomical finding that approached clinical significance was a frank disk herniation, while depression was the only factor that was actually found to be a significant predictor of future episodes of LBP.
Even though there is evidence that asymptomatic findings are the norm with imaging and may not be predictive in the development or prognosis of LBP, could there be any dangers with imaging above and beyond the cost and potential exposure to radiation? A number of studies have identified that, all other things being equal, patients receiving imaging for LBP show no difference or even worse outcomes than those randomized to not receive imaging. For example, studies consistently show associations between increased use of imaging and higher rate of spinal surgeries and injections, consequently putting patients at risk for prolonged disability and complications including death5,6. Another study found that patients randomized to receive their MRI results had worse health perceptions compared to patients not given their results7.
Current evidence-based clinical practice guidelines advise clinicians to avoid routine imaging for non-specific LBP, except to rule out serious pathology (1-2%) and patients with progressive neurological deficits8. In a meta-analysis reviewing randomized controlled trials of early imaging for non-specific LBP, there were no identified red flag conditions that were missed secondary to not imaging patients9. Future directions should look to provide specific protocols for lumbar imaging, similar to the well established Canadian Cervical Spine Rules10. Until then, evidence from large population based studies advocates for early physiotherapy intervention as this has been associated with improved patient outcomes when compared to patients who receive delayed referral for physiotherapy services11, 12. Furthermore, early physiotherapy also translated into a reduction in overall healthcare costs, opiate based medication usage and invasive procedures that carry greater risk of significant side-effects.
Clinical Bottom Line: Patients presenting with non-specific LBP should not receive routine medical imaging. These patients may benefit from early physiotherapy that includes active based treatment and reassurance of a favourable prognosis.
Authors:
STEVE YOUNG, BSCPT, BA
SEAN OVERIN, BHK, MPT
References
1. Lawrence RC, Helmick CG, Arnett FC. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis & Rheumatism 1998; 41:778-799.
2. Casazza, BA. (15 February 2012). "Diagnosis and treatment of acute low back pain". American family physician 85 (4): 343–50
3. Jensen, Maureen C., et al. "Magnetic resonance imaging of the lumbar spine in people without back pain." New England Journal of Medicine 331.2 (1994): 69-73.
4. Jarvik, Jeffrey G., et al. "Three-year incidence of low back pain in an initially asymptomatic cohort: clinical and imaging risk factors." Spine 30.13 (2005): 1541-1548.
5. Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonance imaging vs radiographs for patients with low back pain: a randomized controlled trial. JAMA. 2003;289:2810-2818.
6. Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine 2003; 28: 616–20
7. Ash, L. M., et al. "Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain." American Journal of Neuroradiology 29.6 (2008): 1098-1103.
8. Chou, Roger et al. 2007. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society.
9. Flynn, Timothy W., Britt Smith, and Roger Chou. "Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good." journal of orthopaedic & sports physical therapy 41.11 (2011): 838-846.
10. Stiell, Ian G., et al. "The Canadian C-spine rule for radiography in alert and stable trauma patients." Jama 286.15 (2001): 1841-1848.
11. Gellhorn, Alfred Campbell, et al. "Management patterns in acute low back pain: the role of physical therapy." Spine 37.9 (2012): 775.
12. Fritz, Julie M., et al. "Primary care referral of patients with low back pain to physical therapy: impact on future health care utilization and costs." Spine 37.25 (2012): 2114-2121.



