The Hurdles of Cognitive Biases
As humans we are forced to navigate our way through a natural and social world that is infinitely complex. So how do we do it? How do we make sense of the complex world in front of us every day? We develop efficiencies. Our brain is evolved for recognizing patterns and these short cuts serve us well in life. But pattern recognition and efficient (“short cut”) thinking isn’t without it’s draw backs; namely cognitive biases! These are the glitches in our thinking that are the hurdles in the path of rational thought. So, are these relevant to physical therapy? You better believe it – these are the hurdles in the path of clinical reasoning.
So what are some of these clinical reasoning “land mines?” Consider what follows, not as an inclusive list, but as an exposure to some cognitive biases that play a roll during clinical encounters.
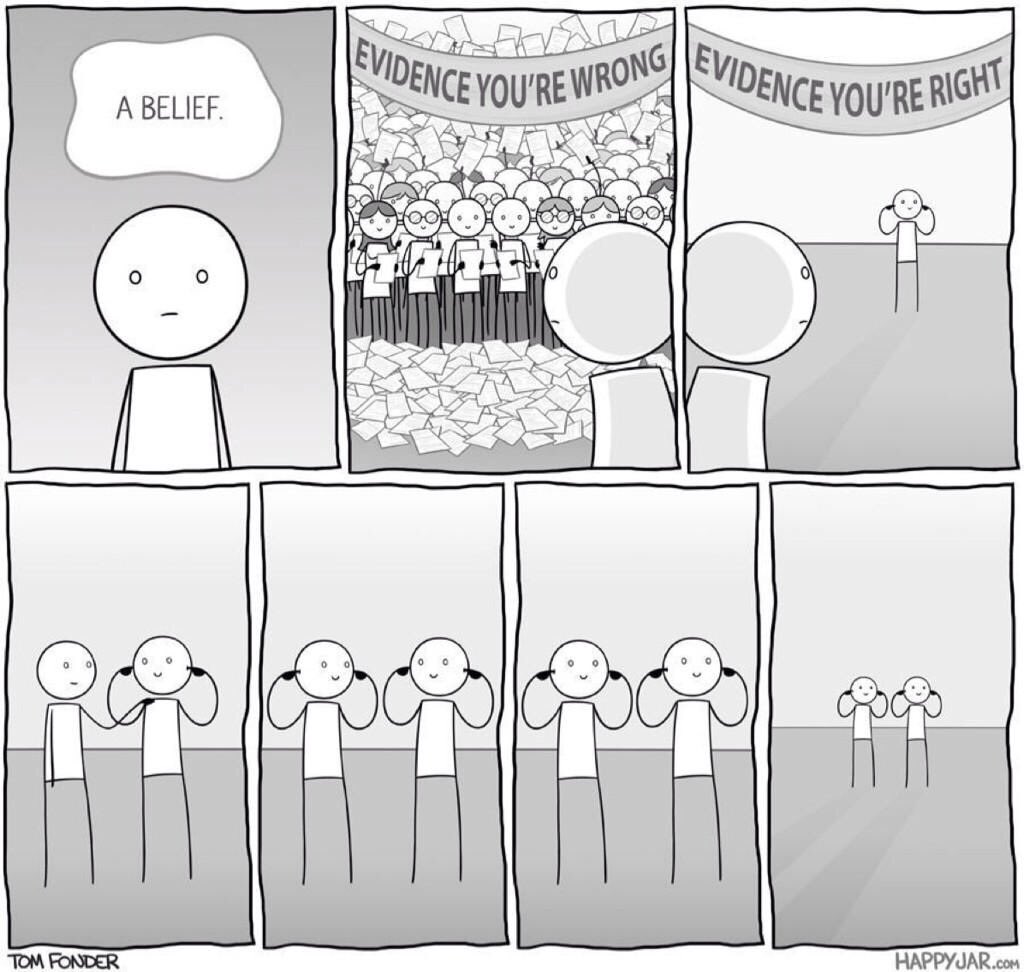
Confirmation bias – gravitating towards information that supports our beliefs.
In my opinion, this is likely the biggest cognitive bias that influences us in clinical practice. It is a large component that leads to the heavy and sometimes nasty debates on treatment methodology between practitioners. Examples of this include “cherry picking the literature” to support your clinical reasoning biases; or “Cave man reasoning” where we think some thing is wrong (i.e. an SI joint that is “out”), which leads to a treatment choice (i.e. lumbopelvic manipulation) that works (i.e. the patient has less pain and moves better) therefore you conclude “I was right!” (“The SI joint was out!”). Here you would have jumped to a conclusion without considering the multitude of possible reasons the treatment might have worked, and the more it works the more this belief becomes entrenched. If you will indulge my soap box moment, here is the problem with that last example: if we fall victim to this “cave man reasoning” and talk about things being “out,” “stuck” or “needing to be put back in,” we run the risk of contributing to iatrogenic MSK issues for patients (read this blog for more).
Pattern recognition is an enormous part of clinical medicine and it’s typically what differentiates a novice from expert clinician (Ref). However, this doesn’t mean you have blinders on. In an excellent perspective paper Dr. Pines discusses the role of confirmation bias in emergency medicine (ref). He concludes with words that we should keep in mind every day:
“Using and teaching metacognition and an understanding of error theory and cognitive forcing strategies may be helpful in minimizing confirmation bias. When the initial clinical impression is not corroborated by objective data, [emergency physicians] must be open to revisiting the possibility of an inaccurate diagnosis and may have to start again…”
Selection bias – when you see the car you just bought everywhere – in PT this is taking a course and suddenly all your clients fit the criteria for the new technique you just learned. And everyone seems to get better with the technique… at first. Eventually, fewer and fewer people seem to fit the criteria. In essence, this is the bias that has us noticing “things” that we are most interested in at that time… these “things” were just as prevalent before we became interested in them, but now that we are aware it seems that these “things” are everywhere … I would offer that, clinically, we look for what we can treat. Being exposed to different ideas, assessments and treatments allows us to look at more of the whole patient presentation. Just remember that the thing you are most interested in currently influences how you see your patient’s presentation, and what you decide to do with them.
Current moment bias – the tendency for humans to choose what is instantly rewarding rather than what is better in the long term – Consider your answer to this question as an example, “would you want $80 now or $100 one year from now?” In PT this bias most often takes the form of focusing on “magic hands” techniques to feel good now, rather than the long term gain of exercises. Both patients and clinicians are guilty of this, as seeing quick change as intoxicating. However, let’s not get so focused on the here and now, that we lose sight of the ultimate goal – an independent patient, that knows how to achieve their goals without our continued involvement.
“if you are doing things right, you should be embarrassed of how you were treating patients when you look back 5 years from now”
Status-Quo Bias – This is what makes changing our clinical habits so hard. This is the adage of, “if it ain’t broke, don’t fix it” that leads us to continue with our habits such as ordering the same food at the same restaurant or using the same “cookie cutter approach” to treatment, because it has worked in the past. If we are to move our profession forward, and provide the best care to our patients, we must challenge the status-quo and traditional thinking! In a recent conversation I had with some colleages one of them said, “ if you are doing things right, you should be embarrassed of how you were treating patients when you look back 5 years from now.” Our evidence based world of physiotherapy is changing rapidly, and we should be striving to adapt to what the new and best science has to offer.
So how do we confront these cognitive biases?
1.Know they exist – you can’t work on what you don’t know. The list above is just a start. Being aware of what biases you are subject to during a clinical encounter is an important part of reflective practice; and simply put – necessary for us to get better.
2.Challenge your biases – personally I know that I am biased toward pain science reasoning, but have started to look at some biomechanical research on patient presentations. While it is hard for me not to be skeptical as I read these articles, at least it has me challenging my bias regularly. Staying on top of current evidence is an excellent way to challenge your biases, but don’t let the status-quo bias lead to this:
This is both status-quo and confirmation bias at work
Here is an article that challenged my use of dry needling with shoulder pain (ref) – the end result was that when added to evidence based care (i.e. manual therapy and exercise directed at the glenohumeral and scapulothoracic joints) dry needling didn’t improve outcomes. A recent study revealed the same result for acupuncture being added to exercise for shoulder pain (ref). These studies have forced me to re-evaluate my use of dry needling for shoulder pain presentations.
3.Develop alternate hypothesis and test them – This one is particularly important to clinical reasoning, and what is so great about the test-re-test method of treatment – test if you made a difference immediately (as long as you maintain your objectivity and don’t talk your self into thinking it is better – this is “choice-supportive bias”). To avoid pit falls in our thinking, we should strive to have systems that have objective checks and balances built-in. This is the scientific method in action in your clinic – trying to disprove your differential diagnosis, or testing if your client really responds to that specific exercise, or just exercise in general.
4.Think about how you think – this is called meta-cognition, and is at the heart of reflective practice. This pairs with knowing which cognitive biases you are susceptible to, but it also goes deeper and asks, “what is influencing your thoughts as you interact with your patient?” For example, did you get enough sleep last night, enough to eat on a busy clinical day, were you able to leave your personal stresses at the door when you interact with your patients. These questions challenge us to be our best selves for our clients. Reflective practice is a skill and gets better with practice!
The take home message is challenge yourself to be better, challenge your biases. Be sure that your reasoning is on sound footing, or where it may be on thin ice. Finally, “be like water,” and be malleable. Make changes in your reasoning that benefit your patients and not your biases! This is the reason for evidence based practice - to be better for our patients.
Educate. Encourage. Empower.

CURTIS TAIT, BSC, MPT, IMS


