Ignoring the Evidence: What can we do about it? (Part 2)
In part 1, we learned that there is a body of evidence that suggests that we have a very hard time accepting evidence that challenges our core beliefs. The Coles notes are:
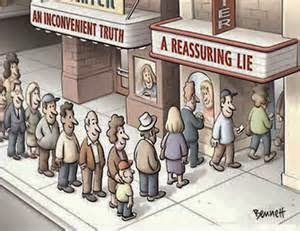
When presented with new evidence on a topic, we chose to evaluate information contrary to our beliefs with more scrutiny.
We more readily accept information that confirms biases, and the stronger we believe something, the more rigorously we do this.
We discussed how relevant this is to patient and colleague education on best evidence.
This also seems very familiar to those clients that simply hear what they want to hear during your education. Easily accepting the parts of your education that confirms their beliefs, and seemingly ignoring aspects that are not in line with their worldview about their pain. To me this brings home the importance of asking the patient, “What do you think is going on? What do you think will help?” It also is the reason why we should be asking a question like, “how will you explain what we talked about to your family,” to identify their understanding. If you don’t ask, you don’t know what understanding they have.
So we all have these processes running when viewing the evidence, it is a natural part of being human. As such, we should not be surprised when our “brilliant” evidence based argument debunking someone else’s “mis-informed” view of the world (e.g. why they have pain, or how treatment actually works) fails to find its mark. With changing core beliefs being so challenging, is there anything we can do to sway people with evidence based reasoning? Two authors in this area of psychology, John Cook and Stephan Lewandowsky, have put out “The Debunking Handbook” to help us avoid making blunders, and improve our success in debunking beliefs. Here are a few highlights:
“keep in mind that people prefer an incorrect model over an incomplete model, and in the absence of a better explanation, they opt for the wrong explanation”
Be aware of, and try not to “trigger,” backfire effects:
Familiarity backfire - mentioning the myth you are debunking can strengthen the myth.
Overkill backfire - using too many arguments against a myth can strengthen the myth belief – “information deficit” model of education.
Worldview backfire - debunking one’s worldview or identity can be threatening, and can strengthen the myth being debunked.
Focus on a few key facts, not the myth. If you must mention the myth, be sure to give explicit warning that the information is false.
A 2011 study (ref) demonstrated that explicit warning about mis-information combined with an alternative explanation was most effective in decreasing subjects reliance on mis-information over general or explicit warnings alone. Provide an evidence informed alternative explanation to what the mis-information is trying to explain.
Studies (ref, ref) have shown that, “when people hear misinformation, they build a mental model, with the myth providing an explanation. When you debunk the myth, you leave a gap in their mental model. When dealing with this problem, keep in mind that people prefer an incorrect model over an incomplete model, and in the absence of a better explanation, they opt for the wrong explanation” (ref).
Graphical information is more effective in debunking then text information.
People provided with graphical surface temperature data correctly concluded that global warming was occurring regardless of their prior beliefs on the subject (ref).

Obviously it is difficult to implement all of these suggestions in the clinic, but we need to utilize this evidence for ourselves if we are to make changes in beliefs during our clinical debunking encounters. This means that you are NOT ALLOWED to easily accept the information in this blog as something you already do. I implore each of us to really reflect on how we can improve our delivery of 'contra-information'.
In our attempts to move physical therapy forward, we often find ourselves “battling” each other in the clinics or online. If we are ever to move past our own echo chambers we should consider applying the above tools from the psychology literature, and try to bring an understanding spirit to the complexity of human communication!
And for our patients, we must use these lessons of human behaviour to help them move past the mis-information holding them back. As a beautiful example of a “play book” for this process in action I refer you to an open access perspective paper by Louw and colleagues (2015) – “The clinical application of teaching people about pain.” The author’s provide excellent examples of evidence based alternative explanations for pain, using graphical information, and advocate graded exposure to pain neuroscience focusing on key facts – i.e. hitting the key concepts of successful debunking.
I am an advocate for effective and evidence based education of our patients and colleagues, and I encourage all of us to make these subtle, but powerful, changes to how we educate. Make your efforts count!

CURTIS TAIT, BSC, MPT, IMS

