Biomechanics Vs. Pain Science (Part 2)
Let's pick up where we left off in Part 1 and dive right in.
Explaining Pain to Patients – Pain Science OR Biomechanics?
This one is no competition. Pain science is the clear winner here. The largest reason is the nocebic effects biomechanical explanations can have on patients. There will be times that we have to minimize sensitizing factors such as a movement direction for a short period, but explaining this via some internal patho-anatomy resulting from some biomechanical fault can create more sensitization from fear and perceived fragility. A qualitative study by Darlow (2013; Ref) found just that:
“Clinicians influenced their patients’ understanding of the source and meaning of symptoms, as well as their prognostic expectations. Such information and advice could continue to influence the beliefs of patients for many years. Many messages from clinicians were interpreted as meaning the back needed to be protected. These messages could result in increased vigilance, worry, guilt when adherence was inadequate, or frustration when protection strategies failed.”
As an example of how much this may impact someone, consider this brief story from one of the CLBP subjects in the study: “Basically all I’ve kind of been told to do by physios is to work on my core...I’ve been tested by various different physios, and Pilates, and I’m apparently ridiculously weak.... I had an abortion because I didn’t think I could have a baby. I didn’t think I could handle it...carrying it, and having extra weight on my stomach (CLBP11).”
On the flip side, these authors noted that, “Clinicians could also provide reassurance, which increased confidence, and advice, which positively influenced the approach to movement and activity.” As an example of this positive messages impact, one acute LBP subject mentioned this: “Lots of reassurance from the [doctor]...made me feel like, “don’t panic, you don’t—you know, this is—this is OK, you’ll be fine, it’s not the start of something awful” (ALBP06).”
In no way am I suggesting that there are therapists out there that are intentionally disabling their patients, but I am confident in saying that in our carrier we have all unintentionally done this. The difference here is when we continue to use the clinical “potty mouth” of patho-anatomy, we are not learning from these wrongdoings.
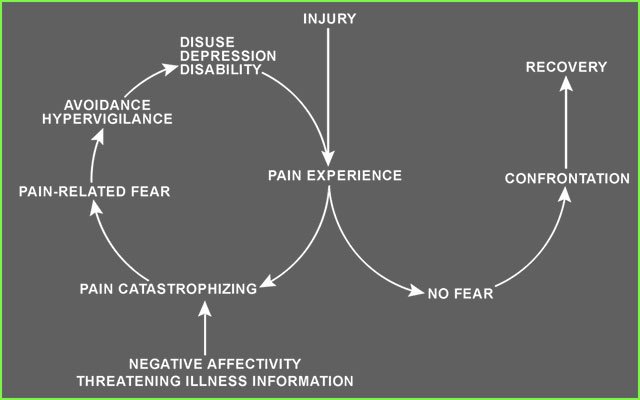
Vlaeyen's excellent representation of two trajectories shaped by the presence or absence of fear. We play an important role in setting the right trajectory.
Over the past 15-20 years we have learned so much about the pain experience, and we can unequivocally say that nociception (i.e. issues in the tissues) cannot be equated to pain. This is to say that just because you have pain does not mean that you have a tissue issue or a problem with your biology (or a problem with your movement). Don’t get me wrong, tissues do generate nociceptive signals, and this is an element in pain perception (and can certainly be the dominant one). However, this is not the end or even the beginning of the story regarding pain perception.
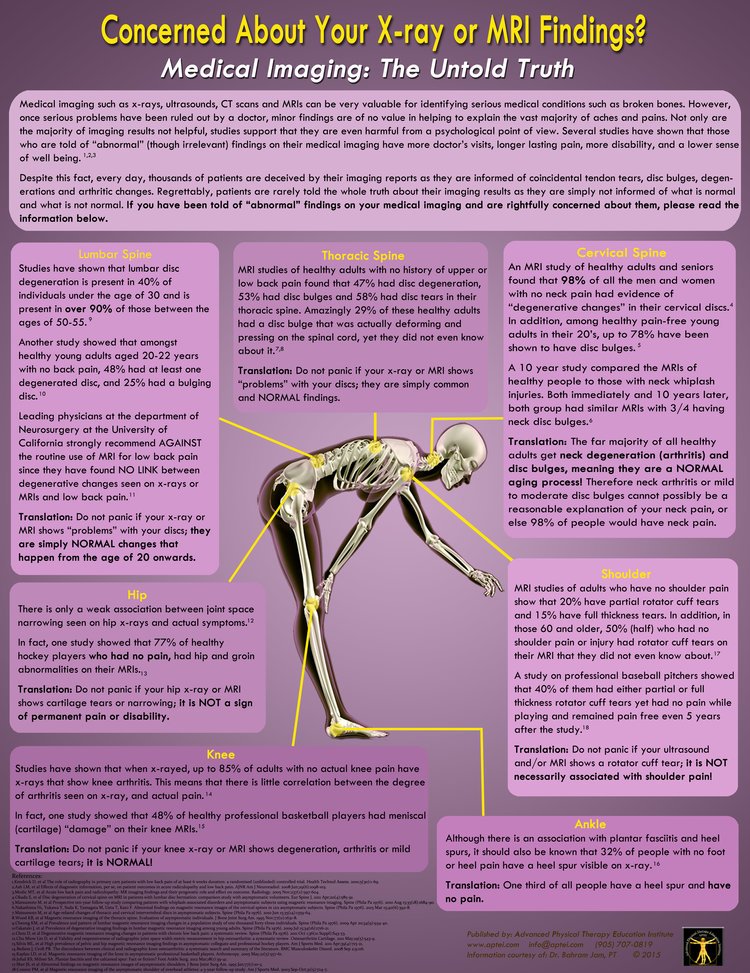
Current research describes a growing awareness that “pathoanatomical changes” (i.e. OA, DDD, bulging discs, shoulder labral tears, rotator cuff tears) are not only common in pain-free populations (Ref, ref), but that focusing on such imaging studies can negatively impact our patients (ref) and healthcare professions (ref). This perspective is compounded by the growing evidence that imaging for common painful MSK conditions does not improve outcomes or enhance treatment when red flags are not present (Ref, ref, ref). All this suggests that the days of pathoanatomy being the focus in MSK medicine should be behind us.
Bahram Jam's excellent poster on medical imaging summarizes some compelling evidence that speaks caution about how to interpret imaging findings.
There is growing support in the literature of the benefits of pain science over traditional anatomy and pathoanatomy focus in MSK medicine for chronic non-specific conditions (Ref, ref, ref, ref). A study by Lee (Ref) demonstrated that for a sample of people with pain lasting longer than 3 months (n = 799) improvements in “pain biology knowledge” over 1 month was associated with significant decreases in pain and improvements in function over one year. This suggests that information on pain science education alone can have a significant positive effect on pain and function over time, and can be a powerful platform to create hope and change for those in pain.
Bridging the clinical divide… My Opinion.
So the larger point here is one you have heard before regarding biomechanics, “don’t through the baby out with the bath water!” However, don’t get confused, the bath water should still go! In this case the “bath water” is purely biomechanical and idealized movement focus of assessment and treatment (people don’t come to physical therapy because their L4 is rotated right on L5 and is lacking cranial glide... even if they say this... especially if they say this). The “baby” that we should be hanging onto is the fact that biomechanics can inform load management, where temporarily decreasing load to calm down sensitivity (whatever might be driving this) may be appropriate, before we start to increase the load incrementally to build resilient tissues and de-threaten movement (I.e. apply stimulus to the highly plastic/adaptable human body). Other times biomechanics may inform how to alter load to demonstrate to a patient that movement is safe (I.e. loaded external rotation of the shoulder at 0 degrees abduction is painful, but at 90 degrees it isn’t), which can de-threaten the painful movement (pain science described modulation of pain perception) and improve the initially painful movement.
“People don’t come to physical therapy because their L4 is rotated right on L5 and is lacking cranial glide... even if they say this... especially if they say this.”
If we continue the analogy, pain science/BPS framework gives us pause to consider the totality of why the baby was having a bath in the first place. Let’s not assume that the baby was dirty and needed a bath... maybe the baby had a fever, or needed soothing, or a multitude of other reasons a baby might be bathed. What I am trying to say is that, by micro focusing on a biomechanical “fault” that needs correcting you are likely missing the bigger picture of what is going on in the person’s life that brought them to you for help (in the end the person has come in because they need help moving forward with an aspect of their life). And worse, that person may leave feeling like they have a new problem, “L4 is rotated to the right of L5 and is lacking cranial glide,” not just that it hurts when they bend over.
Physiotherapists have the amazing opportunity to connect with our patients and help return them to what they love to do in life. This is both a privilege and a responsibility. To honor this, our profession would do best to take the greatest of the old and new evidence, and help our patients focus on the capacity of the human body to adapt and improve! When our patients, community, and greater society learns how resilient their bodies are, we all win!
So throw out the bath water, keep the baby, and get to know why the baby needed a bath in the first place!
Featured
CURTIS TAIT, BSC, MPT, IMS